Infections and Psoriasis
The Link Between Infections and Psoriasis:
How Much Infection Spreads in Psoriasis?
Introduction:
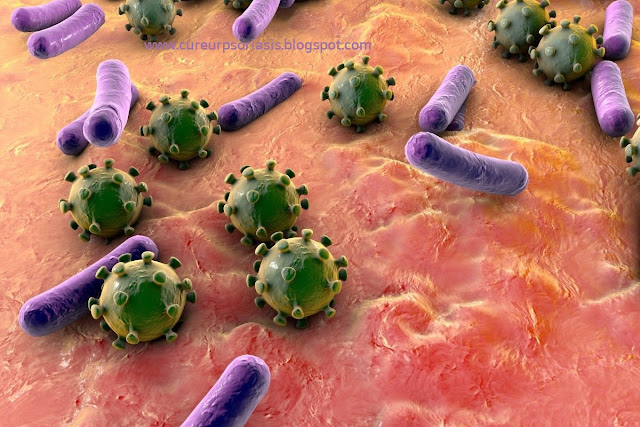
Psoriasis, a chronic autoimmune skin condition, not only affects the skin but also impacts the immune system. As a result, individuals with psoriasis are more prone to certain infections compared to the general population. In this article, we explore the relationship between psoriasis and infections, shedding light on the prevalence, types, and impact of infections in individuals living with this condition. Understanding this connection is crucial for effective management and prevention strategies.
Prevalence of Infections in Psoriasis:
Research indicates that individuals with psoriasis have a higher risk of developing infections compared to those without the condition. The prevalence of infections in psoriasis patients can be attributed to several factors, including immune system dysfunction, compromised skin barrier, and the use of certain medications to manage the disease.
Immune System Dysfunction and Infections:
Psoriasis is an immune-mediated disorder characterized by an overactive immune system. The immune system's constant activation can result in impaired immune responses, making individuals more susceptible to infections. This vulnerability stems from a weakened ability to fight off invading pathogens effectively.
Skin Barrier Impairment and Infections:
Psoriasis often leads to the development of thickened, scaly plaques on the skin, which compromises the skin's natural barrier function. The disrupted skin barrier provides an entry point for bacteria, viruses, and fungi, increasing the risk of skin infections. Common skin infections in individuals with psoriasis include bacterial infections (such as impetigo and cellulitis) and fungal infections (such as candidiasis and tinea).
Streptococcal Infections and Psoriasis:
Streptococcal infections, particularly streptococcal throat infections, have been associated with psoriasis flare-ups. This link is attributed to the body's immune response to streptococcal bacteria triggering an inflammatory response that worsens psoriasis symptoms. In some cases, treating streptococcal infections can lead to an improvement in psoriasis symptoms.
Respiratory Infections and Psoriasis:
Respiratory infections, such as the common cold or flu, can have a significant impact on individuals with psoriasis. These infections can cause systemic inflammation and immune system activation, which can trigger or exacerbate psoriasis flare-ups. It is crucial for individuals with psoriasis to take necessary precautions to prevent respiratory infections, including regular hand hygiene and avoiding close contact with individuals who are sick.
Medications and Infection Risk:
Certain medications used to manage psoriasis, such as immunosuppressants and biological therapies, can increase the risk of infections. These medications suppress the immune system to control the autoimmune response in psoriasis, but they also decrease the body's ability to fight off infections. It is essential for individuals with psoriasis to discuss potential infection risks with their healthcare provider and to monitor for any signs of infection while on these medications.
Impact of Infections on Psoriasis:
Infections can have a significant impact on the severity and progression of psoriasis. When an infection occurs, the body mounts an immune response, triggering inflammation throughout the body. This systemic inflammation can exacerbate existing psoriasis symptoms and lead to the development of new lesions. Additionally, infections can delay wound healing in individuals with psoriasis, prolonging the duration of flare-ups.
Preventive Strategies:
Reducing the risk of infections is crucial for managing psoriasis effectively. Here are some preventive strategies individuals with psoriasis should consider:
a. Maintain Good Hygiene: Practice good hygiene by regularly washing hands, especially before touching the face or affected areas.
b. Protect the Skin: Keep the skin well-moisturized and avoid irritating or harsh substances that may compromise the skin barrier. Proper wound care and prompt treatment of skin injuries are essential.
c. Vaccinations: Stay up to date with recommended vaccinations, including the annual flu shot. Consult with a healthcare provider to ensure the appropriate vaccines are received based on individual circumstances.
d. Minimize Exposure to Sick Individuals: Avoid close contact with individuals who have respiratory or contagious infections, as they can increase the risk of contracting an infection.
e. Communicate with Healthcare Providers: Regularly communicate with healthcare providers to discuss potential infection risks, particularly when considering new medications or treatments.
Conclusion:
Psoriasis is not just a skin condition—it significantly impacts the immune system and can increase the risk of infections. Understanding the prevalence, types, and impact of infections in individuals with psoriasis is crucial for effective management and prevention. By adopting preventive strategies, maintaining good hygiene, and working closely with healthcare providers, individuals with psoriasis can minimize the risk of infections, improve overall health, and better control their condition.











Comments
Post a Comment